Introduction
It is estimated that as many 200,000 patients in the UK suffer with Severe Asthma1, a condition that means they experience frequent asthma attacks, hospital admissions and daily symptoms despite maximal medical therapy. It is a complex condition which may be driven by different inflammatory pathways, but typically severe asthma patients face a substantial burden of illness and marked reductions in quality of life.
Many with severe asthma live with poor asthma control typified by emergency admissions to hospital and regular courses of oral corticosteroids- drugs which can have devastating side effects on physical and mental health. As a result, severe asthma is associated with very high healthcare costs due to medication use, unscheduled healthcare utilisation and management of steroid-related adverse events. These costs have been shown to be four times higher for uncontrolled severe asthma patients than for those with well-controlled asthma2.
The advent of biologic therapies for severe asthma and the formalisation of specialised severe asthma services and networks (“Severe Asthma Services in Adults” – commissioning document A14/S/B) has hugely improved outcomes for patients who are able to access these services. It is estimated that in England over 60,0003 patients currently suffering with severe asthma would benefit from an asthma biologic. However, prescribing data suggests that only ~11,000 of these patients are being treated with biologic therapies.
A recent review of patient journey times to asthma biologics has shown that 60% of patients4 have uncontrolled asthma for over 2 years prior to reaching specialist severe asthma services. Once reviewed in a severe asthma centre, there is variation in the time taken for biologic therapy to be commenced, influenced by both patient related and centre related factors. During this time, the patient is exposed to increasing doses of oral steroids with the risk and incidence of steroid related side effects accumulating.
Aligned with clinical priorities in the NHS Long Term plan on improving outcomes for patients with respiratory disease, the Accelerated Access Collaborative (AAC) Asthma Biologics Rapid Uptake Programme aims to support improvements in pathways and practices to ensure more patients receive timely specialist care for their severe asthma and access asthma biologics.
Background
The rationale for the Accelerated Access Collaborative (AAC) Asthma Biologics Rapid Uptake Programme being that severe asthma currently falls outside of NICE guidelines, and whilst there is guidance and service criteria for elements of the pathway (i.e primary care, tertiary care or biologics prescribing), there is no single guidance document that brings together all parts of the pathway and offer guidance on acceptable timeframes at each stage.
A major ambition of the programme has been to bring together the organisations committed to improving severe asthma care and to agree, by consensus, what optimal care should look like across the entire patient journey. We hope the information collated in this consensus pathway will help guide and inspire systems and regions to rethink the care pathways for the uncontrolled and severe asthma patients they care for. Reflecting the objectives of the AAC Asthma Biologics RUP Programme, this pathway focusses on biologic therapy. However, we recognise that the management of patients with uncontrolled and severe asthma may require a range of approaches. This pathway is aimed at supporting the care of adults (age ≥18 years) with uncontrolled and severe asthma.
Importantly, this is not a mandated approach, as pathways for this unique group of patients need to be assessed in the context of wider asthma services at system level. Commissioners are encouraged to take into consideration other factors such as the local patient population, potential sources of health inequalities, workforce and the healthcare landscape. This pathway contains resources and recommendations on how to deliver optimal care for patients with uncontrolled and severe asthma at a local level. We hope that this pathway will be useful whether your role is in clinical care, service management, service administration or commissioning to shape local discussions and redefine asthma pathways.
To complement the adoption and implementation of the Consensus Pathway the AAC have produced a suite of educational resources that will be helpful for clinicians involved in the care of patients with uncontrolled and potentially severe asthma.
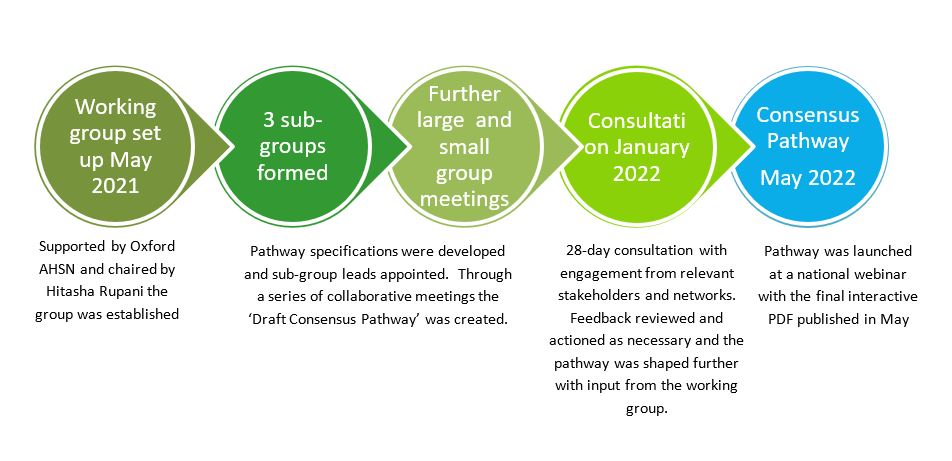
Building Consensus
References:
- Slipping through the net, Asthma UK, 2018, and, Living in Limbo, Asthma UK, 2019
general population, Overview of attention for article published in Thorax, September 2017
- NHSE BlueTeq data 2021
- A review of the patient journey to biologic initiation in UK severe asthma centres, written by
Lottie Renwick, Asthma UK and the British Lung Foundation, Dr Hitasha Rupani, University
Hospital Southampton NHS Foundation Trust and Andrew Cumella, Asthma UK and the British
Lung Foundation, December 2021